THE GLENROSE REHABILITATION HOSPITAL (GRH)
The Glenrose Rehabilitation Hospital (GRH) is the largest free-standing, comprehensive tertiary rehabilitation hospital in Canada, serving patients of all ages who require complex rehabilitation to enable them to participate in life to the fullest. The 244-bed facility provides specialized physical rehabilitation and therapeutic services across 16 professional disciplines and offers both inpatient and outpatient services. Complex rehabilitation approaches at the GRH are supported by cutting-edge research and innovation, technology development and academic teaching. The GRH is part of Alberta Health Services (AHS), Canada’s largest province-wide, integrated health system, which is responsible for delivering health services to more than 4.4 million people.
As a leading tertiary rehabilitation hospital, the GRH embraces innovation as a core feature of its activities. The need to support rehabilitation innovation has never been greater. One in five Canadians has a physical or cognitive disability, and growing demand for virtual or remote healthcare has been prompted by the rapid emergence of the COVID-19 pandemic and the ensuing adoption of lockdowns that has changed the health care delivery model. Outpatient rehabilitation services are also experiencing high demand due to factors that include higher survival rates of people with critical health issues, the trend in health care to discharge patients back to the community as early as possible, and a growing demand by older adults to age-in-place.

THE GLENROSE HOSPITAL FOUNDATION (GHF)
A major supporter of rehabilitation innovation is the Glenrose Hospital Foundation (GHF). Established in 1994, the GHF collaborates closely with donors and stakeholders to secure funding for projects aimed at re-imagining human ability. The GHF mobilizes resources to accelerate advances in human ability and, through strategic investments in translational research and innovation, is helping to shape the future of rehabilitation.
“We’re forging ahead with technology-enabled healthcare — powered by donors who have a passion for advancing patient outcomes and making specialized rehabilitative care even more accessible to those who need it most.” — Mark Korthuis, President and CEO, The Glenrose Rehabilitation Hospital Foundation
A recent GHF investment is in brain computer interface technologies, an emerging and promising access technology for patients with complex physical needs such as cerebral palsy, spinal muscular atrophy, brain injury, spinal cord injury, or stroke.

CLINICAL INNOVATORS AT THE GLENROSE DR. JACQUELINE HEBERT
Limb amputation is a life-altering event affecting mobility, quality of life, and participation in daily activities. In Alberta alone, over 450 individuals undergo major lower limb amputations every year. Under the leadership of Dr. Jacqueline Hebert, the Bionic Limbs for Improved Natural Control (BLINC) Lab brings together a diverse group of inter-disciplinary researchers interested in collaborative research to improve limb function after amputation, from surgical techniques to device development, motor control, and sensory feedback. Her research group has a history of pioneering achievements in the field of prosthetics and improving the lives of Canadians living with limb amputation.
Most recently, Dr. Hebert has brought osseointegration to Alberta Health Services with the support of the GHF and the University of Alberta Hospital Foundation. Osseointegration is an innovative new procedure that completely bypasses the need for a prosthetic socket. The conventional method following a lower-limb amputation uses a hard-shell socket that is fitted over the remaining limb. The hard shell is uncomfortable and can lead to poor fit, skin breakdown, and poor control of the prosthesis. With osseointegration, the surgeon inserts a titanium implant into the remaining thigh bone, which stays there permanently and—over time—naturally integrates with the bone. This implant extends through the skin and allows a direct structural connection to the external prosthesis. The success of osseointegration depends on using specially designed titanium implants, careful surgical techniques, and a controlled period of specialized rehabilitation.


There are many benefits of prosthetic devices attached directly to the bone by an osseointegrated implant, which include: increased stability and secure attachment of the prosthesis; better range of motion at the hip; improved bone health; improved awareness of the position of the prosthesis; and patients can put on and take off the prosthesis faster. These benefits increase patient comfort when sitting, reduce the energy required to walk and allow patients to wear the prosthesis for longer periods daily, which greatly contribute to an improved quality of life.

DR. LONNIE ZWAIGENBAUM
Dr. Lonnie Zwaigenbaum is a pediatrician at the GRH, Director of the Autism Research Centre, Stollery Children’s Hospital Foundation Chair in Autism and Professor in the Faculty of Medicine & Dentistry at the University of Alberta.

His research focuses on early development in autism spectrum disorder (ASD) and related neurodevelopmental disorders. With the goals of identifying early behavioral and neurobiological markers of ASD, his research group is following a high-risk cohort; namely, infant siblings of children with ASD. This is helping the group identify specific risk markers to aid in earlier diagnosis and study basic processes (e.g., attention, emotion, executive control) that may underlie later symptoms.
Dr. Zwaigenbaum and his team have developed the first observational measure designed to detect signs of ASD in six to 18-month-old patients. This measure can be completed by parents as a questionnaire, which is effective in identifying infants diagnosed with ASD as early as 6 months of age. This innovative measure has been highlighted by the Canadian Institutes of Health Research as a significant Canadian health research achievement and has been adopted by numerous groups and networks internationally for improving the early detection and diagnosis of ASD and informing development of new interventions for toddlers with early signs of ASD. Dr. Zwaigenbaum is currently researching a novel training and mentoring approach with community pediatricians to improve diagnostic capacity and access and ongoing health care to children with ASD.
DR. MING CHAN
Dr. Ming Chan is a rehabilitation medicine specialist at the GRH and professor of Physical Medicine and Rehabilitation at the University of Alberta. His clinical practice is in neuromuscular disease, with his research focusing on peripheral nerve regeneration, myoelectric prosthetic control, and neurodegenerative disorders.

Dr. Chan observed in his practice that shoulder movements are frequently compromised, not just from nerve damage causing muscle loss but also from associated bony or soft tissue shoulder injuries. This can be highly debilitating for individuals, not just in limiting daily activities, but also from pain due to a frozen shoulder. Existing treatment options are limited and often expensive, and while static braces are available, they only provide support to the arm in a fixed position.
To address these limitations, Dr. Chan developed the dynamic shoulder brace (DSB) to assist individuals with peripheral nerve injuries to perform shoulder motions: adduction, abduction, horizontal flexion, internal and external rotation.

Incorporating continuous design improvements using patient feedback, Dr. Chan modified a common socket wrench to replicate the shoulder joint’s adduction abduction motion to replace the commonly used internationally sourced Ottobock locking joint, which also significantly reduced the cost. Dhruvi Dave, a University of Alberta co-op student in mechanical engineering, assisted Dr. Chan in developing the rachet mechanism. Dr. Chan received funding from Campus Alberta Neuroscience to patent the invention and support from the GRH to undertake clinical trials with patients and further develop the product.
The DSB is comprised of a body shell and an arm cuff custom fitted to the individual. The ratchet hinge joint, inserted in a lightweight low profile Teflon housing mounted on the body shell, allows the arm to be locked into place at any angle up to 90 degrees. This allows the arm to be positioned through a range of movements in front and to the side of the body. Once the activity is completed, the patient can lower the arm by pulling on a strap connected to the ratchet hinge joint in a controlled manner. The DSB helps in reducing patient recovery time and allows for more functional movement while individuals are performing activities of daily living.
GLENROSE REHABILITATION RESEARCH, INNOVATION AND TECHNOLOGY
Innovation at the GRH is supported through Glenrose Rehabilitation, Research, Innovation & Technology (GRRIT), which develops technical solutions for challenges experienced by practitioners and people living with physical or cognitive disabilities and champions the commercial application of clinical research. GRRIT supports industry in accessing clinical facilities, offers expertise in business development, engineering, rehabilitation sciences, product design, development, validation, adoption, and implementation and assists industry in recruiting highly qualified personnel.
GRRIT works closely with the GHF and external partners that include Prairies Economic Development Canada (PrairiesCan), Scoliosis Alberta, Faculty of Engineering at the University of Alberta, Schulich School of Engineering at the University of Calgary and Alberta Innovates. Support from external partners allows GRRIT to bring industry into the clinical setting to accelerate applications for rehabilitation technologies, to recruit and train students and to make a major contribution to strengthening provincial capabilities to develop and commercialize health-related innovations. One example is the collaboration between the GRH and Calgary’s Foothills Medical Centre (FMC) to support a clinical technical lead position at FMC who is working closely with clinical technology leads at the GRH.
STUDENT INNOVATION AT THE GLENROSE
Clinicians and students are an integral part of innovative activities at the GRH. GRRIT facilitates opportunities for clinicians and students to participate in research and innovation activities and to work with industry partners and engage in new product developments. Additionally, GRRIT helps to coordinate co-op student projects based on clinical challenges encountered by GRH front-line clinicians which include nurses, occupational therapists, physical therapists, and speech pathologists. Students develop and apply their technical and project management skills through working with front line staff to solve clinical problems and producing practical prototypes which can be evaluated by clinicians and patients. One example is the Light Board Project, a novel technology idea which originated in the pediatrics department at the GRH. The goal of the technology is to assist with upper extremity gross and fine motor rehabilitation, but in a fun and child-friendly way. This extended size model, on a 5’ x 3’ height and angle adjustable board, was inspired by the traditional notebook sized ‘Lite Bright’ game. The size of the Light Board allows for large arm movements, while the various styles and colors of peg help children with limited dexterity to improve their fine motor skills by using pegs with varying grip techniques.
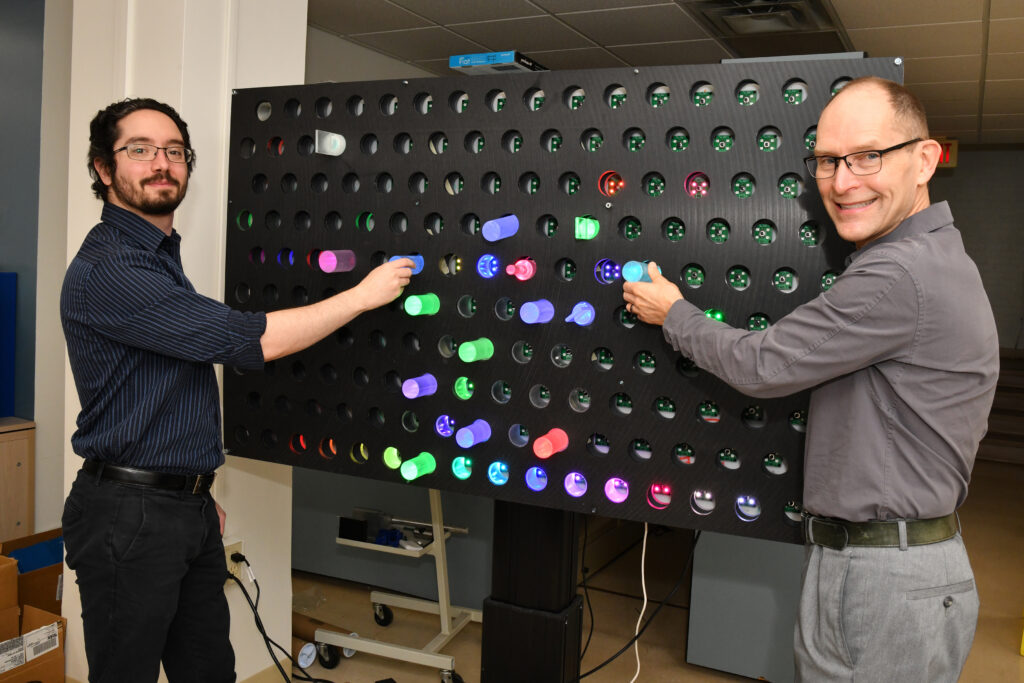
The original prototype was designed and fabricated by a Bachelor of Technology capstone team from the Northern Alberta Institute of Technology (NAIT) before being passed on to University of Alberta engineering co-op students, who are finalizing the design and manufacturing of the pegs before deploying the Light Board for clinical use. Successful development of the Light Board would not be possible without ongoing engagement between front line therapists, students, patients and GRRIT staff to undertake multiple revisions to the original idea.

Jade Belisle, a University of Alberta mechanical engineering co-op student (biomedical specialization), is preparing for a print job using the Phrozen Sonic Mega 8k resin 3D printer. 3D printing is used extensively for prototype development of innovative devices at the GRH that can improve the lives of patients during their rehabilitation journey.

Steven Phan is a University of Alberta biomedical engineering masters student, working on cutting edge indoor tracking systems to assess and monitor older adults in their homes. Technologies like ultra-wideband (UWB) have the potential to transform how cognitive and functional assessments are done, enabling clinicians and family members of patients to optimize home care using real-life data. Steven is also working with the Program to Accelerate Technologies for Homecare (PATH), a national research and testing initiative involving the GRH, University of Alberta and related health facilities and universities in Toronto, Waterloo and Ottawa.
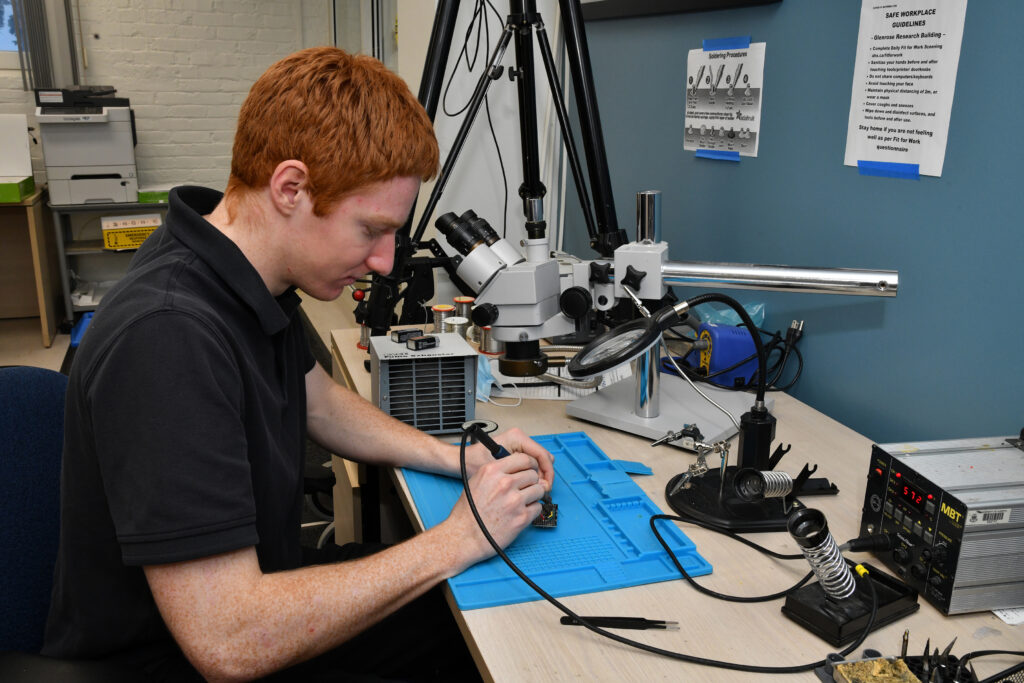
Quin Greenaway, a University of Alberta electrical engineering co-op student, is adding electronic components to a circuit board. Quin is building on his software and hardware expertise for the development of a low-cost surface EMG biofeedback system which may be used for home training. Patients with nerve transfers will use this device to help restore upper extremity function by providing visual feedback while performing tasks to re-learn techniques for reliable muscle activation.
INDUSTRY INNOVATORS AT THE GLENROSE
KARMED
Upper extremity function plays a critical role in completing activities of daily living, employment, and participating in recreational activities. The flexion, extension, pronation, and supination – FEPSim® device is a device for hand and wrist rehabilitation that can be adjusted according to the patient’s requirements in rehabilitation. The FEPSim® can also be used to assess the patient’s strength and range of motion of the forearm, wrist, and hand.
The original concept of the FEPSim® developed from a project involving NAIT capstone students and therapists at the GRH. Therapists had identified the need to address the high number of disabilities related to the hand, wrist, and forearm, and the clear lack of progressive rehabilitative devices. KARMED was drawn into the project, given their expertise in advanced manufacturing through its parent company, Karma Machining and Manufacturing. GRRIT helped KARMED recruit University of Alberta engineering co-op students to further assist in product development.
Robert Hirsche, an occupational therapist at the GRH and one of GRRIT’s clinical technical leads, worked closely with Darryl Short at KARMED in facilitating clinical feedback to develop the device. Dr. Antonio Miguel Cruz, GRH Research Affiliate, Associate Professor in the Faculty of Rehabilitation Medicine and director of the Product Evaluation and Applications Research (PEAR) lab at the University of Alberta, led a user feasibility study of the FEPSim® which validated its usefulness as a versatile therapy tool with improved measurement and grading systems and confirmed its wide acceptance by therapists.

“Collectively, we’re a group of hands-on innovators who manage the entire product cycle from prototype iterations through full-scale manufacturing, testing, approvals, and the ever-important user experience.” – — Darryl Short, KARMED Co-Founder
The FEPSim® is now being sold and distributed across North America, allowing patients to simulate daily activities, such as turning a doorknob or using a screwdriver, to strengthen muscles and improve flexibility. The device, developed through collaboration between therapists, students, industry and supported through GRRIT, can treat a wide range of patients recovering from severe strokes, burns and muscle and bone injuries.
BOWHEAD CORPORATION
In 1996, Christian Bagg became a wheelchair user following a snowboarding accident that resulted in a sudden loss of mobility. At the time of the accident, Christian was completing his apprenticeship as a machinist. Following his injury, Christian began to tinker in his workshop, and mobility devices became his focus; it was the beginning of the Bowhead story. Christian was unable to find a manual wheelchair that could accommodate his 6’4” frame and support his mobility needs as a T7-9 paraplegic, so he decided to build his own. Fast forward two decades and Bowhead Corporation, which Christian co-founded, has become a leader in the adaptable mobility market.

GRRIT became involved with Bowhead as the company was developing its first product, the Bowhead ‘Reach.’ Bowhead had identified a severe lack of adaptable mobility options available that allow adults safe access to outdoor movement and activity. Depending on the needs of the individual, this requires options that provide stable safe riding machines that can traverse varying terrain from paved streets and sidewalks to hiking trails in parks.
A large market exists for people with disabilities and seniors who have mobility limitations, and Bowhead sought to address this market by providing a means for individuals with lower limb impairments to access outdoor recreational areas including hiking/bicycle trails. The Bowhead Reach and more recent products, such as the Bowhead RX adaptive cycle, incorporate a unique articulated suspension design that allows individuals to navigate rough terrain safely through an autonomous steering/levelling system.

GRRIT has provided Bowhead with funding for product development and assisted Bowhead in recruiting eight University of Alberta engineering co-op students, who have assisted in product design, development, and assembly. Bowhead recruited one of these students upon her graduation to work full-time as part of their engineering team. GRRIT also assisted Bowhead in securing experienced professional engineering talent to work on product development.
Bowhead is scaling its business and developing new product lines, including a height-adjustable wheelchair and self-levelling mobility scooter. GRRIT is working with Bowhead to establish a provincial mobility cluster that supports local innovators developing new products that improve the lives of people living with mobility challenges.
TRUE ANGLE
True Angle is an Edmonton-based health tech company whose mission is to empower people to live better lives through smart technologies. Company origins can be traced back to Dr. Jana Rieger’s lab at the University of Alberta, when Dr. Rieger, along with her research colleagues Dylan Scott and Gabriela Constantinescu, began to develop a new device to help patients recover from swallowing impairments dysphagia. Approximately one in six adults will experience a swallowing disorder in their lifetime because of conditions such as stroke, cancer, and neurological disorders.
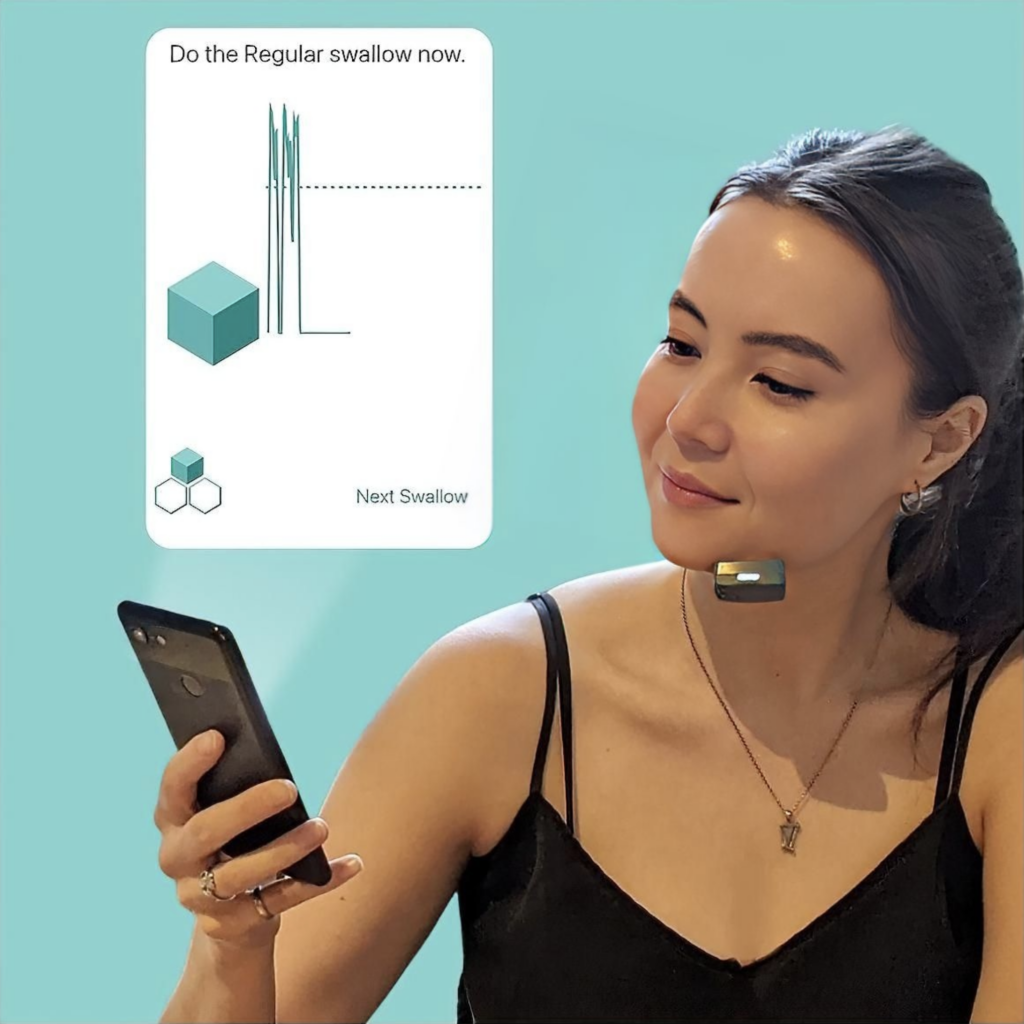
The innovative device, called Mobili-T, short for mobile therapist, is a wireless piece of hardware that senses muscle activity when placed under the chin and gives patients direct feedback about swallowing muscle activation. The device pairs real-time visual biofeedback with a smart software-based coaching system, all while maintaining a direct connection to the speech-language pathologist, who can track a patient’s progress. The software offers a personalized approach by helping people set targets for their daily exercises, through sensing their muscle energy levels and setting realistic goals.
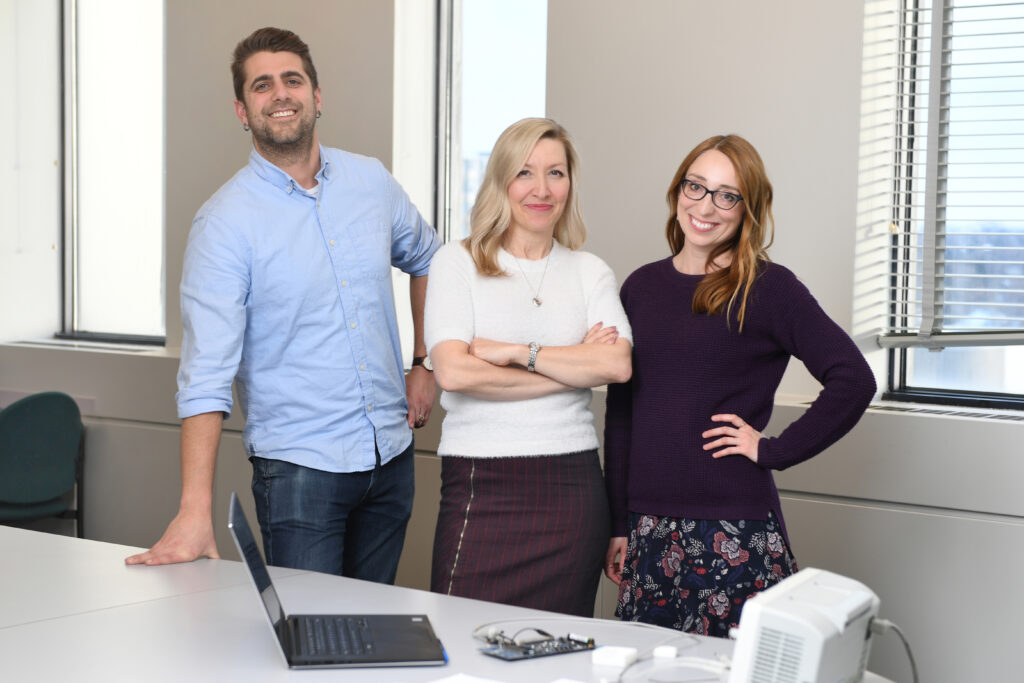
GRRIT assisted True Angle in undertaking usability/feasibility studies to develop its Mobili-T system, assisted in patient recruitment, patient testing and data collection and provided early-stage commercial advice. True Angle has raised over $5 million in investment and
grant funding; their products are now available across the globe. The Mobili-T system addresses a key challenge in swallowing rehabilitation, in that there are never enough trained clinicians to meet the global demand for intensive dysphagia exercise rehab, which can help to prevent the life-threatening side effects of dysphagia that are extremely costly to health care systems. True Angle’s innovation is mobile, easily scalable and the pocket-sized technology allows people to take charge of their health, overcome their swallowing disorders, and improve their quality of life.
NANOTESS
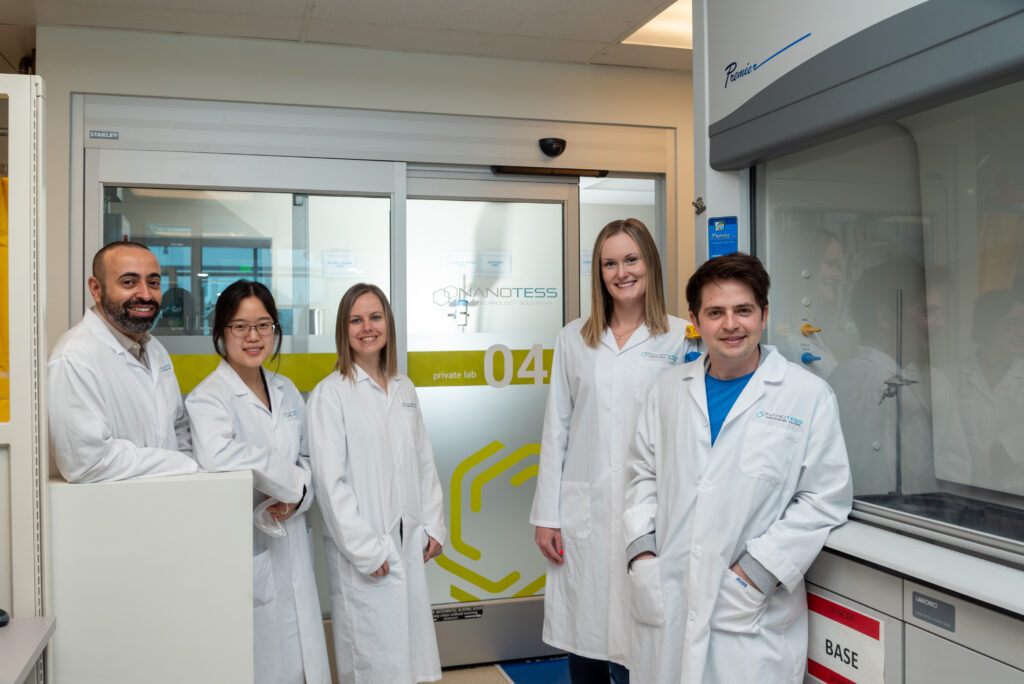
NanoTess is a values-based enterprise, co-founded by Megan Leslie and Julian Mulia, with a vision to “prevent unnecessary suffering through technological innovation.” The company’s focus is on helping patients with chronic wounds such as diabetic foot ulcers and developing products that are accessible and affordable for those who need them. Their team has over 40 years of cumulative experience in material science with particular interest in nanotechnology. Invisible to the naked eye and 1000 times smaller than bacteria, nanotechnology solutions and nanomedicine offer the basis for the next revolution within the health industry.
Nanotess developed their first product, called NanoSALV, which is an antimicrobial gel that is designed as a liquid dressing. The advantage of a liquid dressing is that it moves away from solid dressings and patches that often do not properly fit a wound. NanoSALV facilitates self-healing and re-epithelialization by providing an adequate medium for the natural healing processes to occur. Suitable for chronic wounds, independent studies have validated that NanoSALV technology provides a broad spectrum antimicrobial effect against viruses, yeasts, fungi, and bacteria, including antibiotic resistant bacteria.

GRRIT’s involvement with Nanotess began in 2021, after the company had won the REHAB Innovation to Commercialization (i2C) competition, which provided Nanotess and nine other aspiring rehab tech ventures with mentorship and coaching, culminating in a pitching competition for $100,000 to support the winner’s further commercialization activities. Nanotess is now working with the GRH and AHS to further trial and test their NanoSALV product.