STATUS QUO IN SPINAL SURGERY IS NOT AN OPTION!
No status quo is synonymous with innovation. Innovation must transform the way we deliver care to patients. On one side this has to involve patient-centered improvement by careful listening and precise information. On the other hand, surgical procedures must apply the principle of less is more – apply state-of-the-art techniques, put less energy into unnecessary elements and focus on the patient.

In Belgium, we can always offer specialised care to our patients. However, we must never forget that every patient is also a human being. Not only super-specialist physicians are needed, but also specialists who keep looking for the reasons why this person is suffering at this moment.
During my work as a physician in the tropics (Tanzania), I became a great admirer of the body’s power to recover.
Not every “abnormality” of the back gives rise to complaints. In other words, if someone has back problems, it does not have to be because of a defect that we see on an MRI or CT scan. The challenge then is to find a solution together with the patient. Often this means: more healthy exercise (sports or just walking), doing small daily activities differently, reducing your total sitting time etc. Sometimes a procedure is necessary to get the patient back on track.
In the past years as an orthopaedic surgeon, I have specialised more and more in the treatment of lower back problems. Never forgetting to look at the patient as a human being rather than the illness.
Let’s look at the various innovations Dr. van Schaik has introduced in both the hospitals where he is working.
He has invested in innovation in communication with the patient and the technicalities of surgical procedures

PATIENT COMMUNICATION INNOVATION
Open and transparent advice
In addition to many technical surgical developments (minimally invasive back surgery), I continue to be interested in patient-centred developments, especially with digitisation in mind.
Like our Patient Application, which gives the patients information about their operation and their pre/post-operative course at appropriate times. Through this patient app, we can monitor the patients’ pain score, their activities, their medication use and many other things. The patients themselves have continuous access to all relevant information regarding their diagnosis, intervention and post-operative course.
Goal:
• Provide clear information at the right time
• To inform the patient well in a clear and understandable language
• Reduce the pre and post-operative stress
This application is not a substitute for the regular explanation by Dr. van Schaik, but an addition to allow reflection in the patient’s own environment and time, and in the early days of post operative surgery it allows monitoring from a distance.
Central messages in our application are:
• Eat and drink healthy
• Try to exercise every day for at least 30 min, non-stop at a slightly elevated heart rate: walking/cycling/swimming/…
• Above all, stay positive, surround yourself with open minded and positive people
• Small steps at a time will improve the quality of your life

THE “EXPERIENCE COACH” PROJECT
The surgeon can answer many questions, however, a first-hand patient story is more relevant and is the reason why Dr. van Schaik started the ‘Experience Coach’ project.
We started the patient experience programme in 2021. When a specific operation is required, Dr. van Schaik offers contact with a patient who underwent the same procedure, so inclusive discussions will occur providing insight of outcome and expectation. In other words, more information in addition to what we, caregivers, already do. All these patients form the team of “Experiences Coaches”.

SPINAL OPERATIONS INNOVATIONS
Operation Room Efficiency
Dr. van Schaik’s goal is to maximise resources by minimising unnecessary requirements. Our regular meetings with the surgical teams have the following results:
• Open and direct communication
• Rule out “pointless” actions resulting in more procedures without extra effort
• Reduction in the number of surgical sets meaning: less draping time, significantly shortening changeover time, with minimal patient disturbance
• Shorter total procedure time
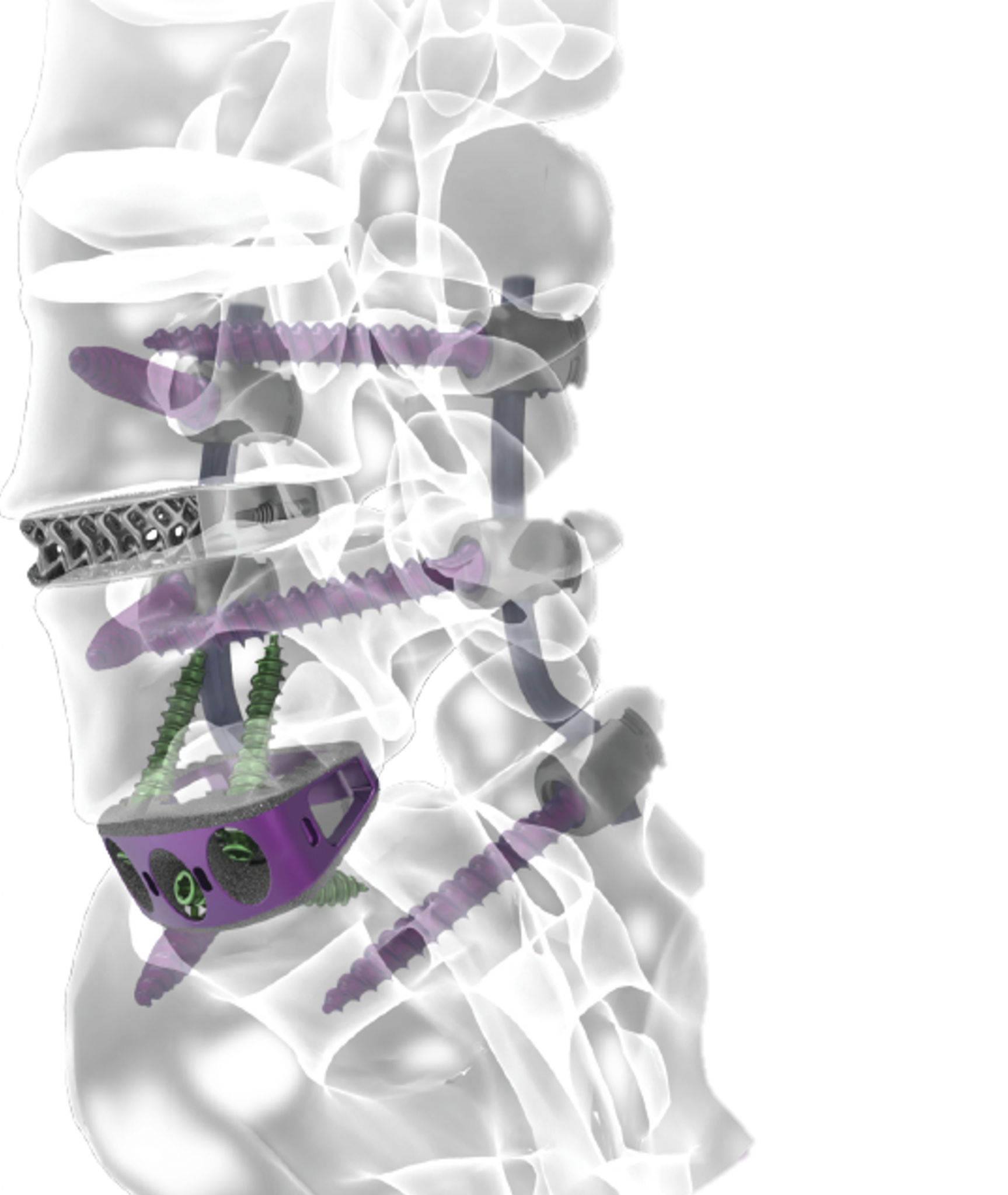
Anterior L5-S1 fusion and lateral L4-5 fusion, percutanius L4-S1 fusion in Single position Surgery
INNOVATIONS IN THE BETTER USE OF EXISTING RESOURCES
The great thing about our profession is that sometimes we can help people with a “simple” tip to sit differently at their desk or to do an additional sport exercise. At other times we perform an operation on the spinal vertebrae in order to get the patient mobile again even better and faster than traditionally.

Anterior view: fusion between the last lumbar vertebrea and the sacrum. Stand alone cage with screw fixation
1. Single Position Technique
Dr. van Schaik was the pioneer in the Benelux to perform a Single Position Surgery on a patient with chronic lower back and leg pain (disc lesion / degenerative disc disease /collapse of the intervertebral disc at L5-S1).
The patient lies on the operating table in the side position and is operated on through a small incision in the abdominal wall. This position provides the surgeon with a precise view of the disc to be operated on. At the end of the procedure, the patient does not have to be turned on their supine position to insert the screws into the vertebrae, we can do it in the same lateral position. Very often a cage with screw fixation in it is sufficient.

Lateral view: fusion between the last lumbar vertebrea and the sacrum. Stand alone cage with screw fixation
This technique considerably shortens operation time thus reducing the period of sedation, ensuring faster patient recovery, less post-operative pain and sooner hospital discharge.
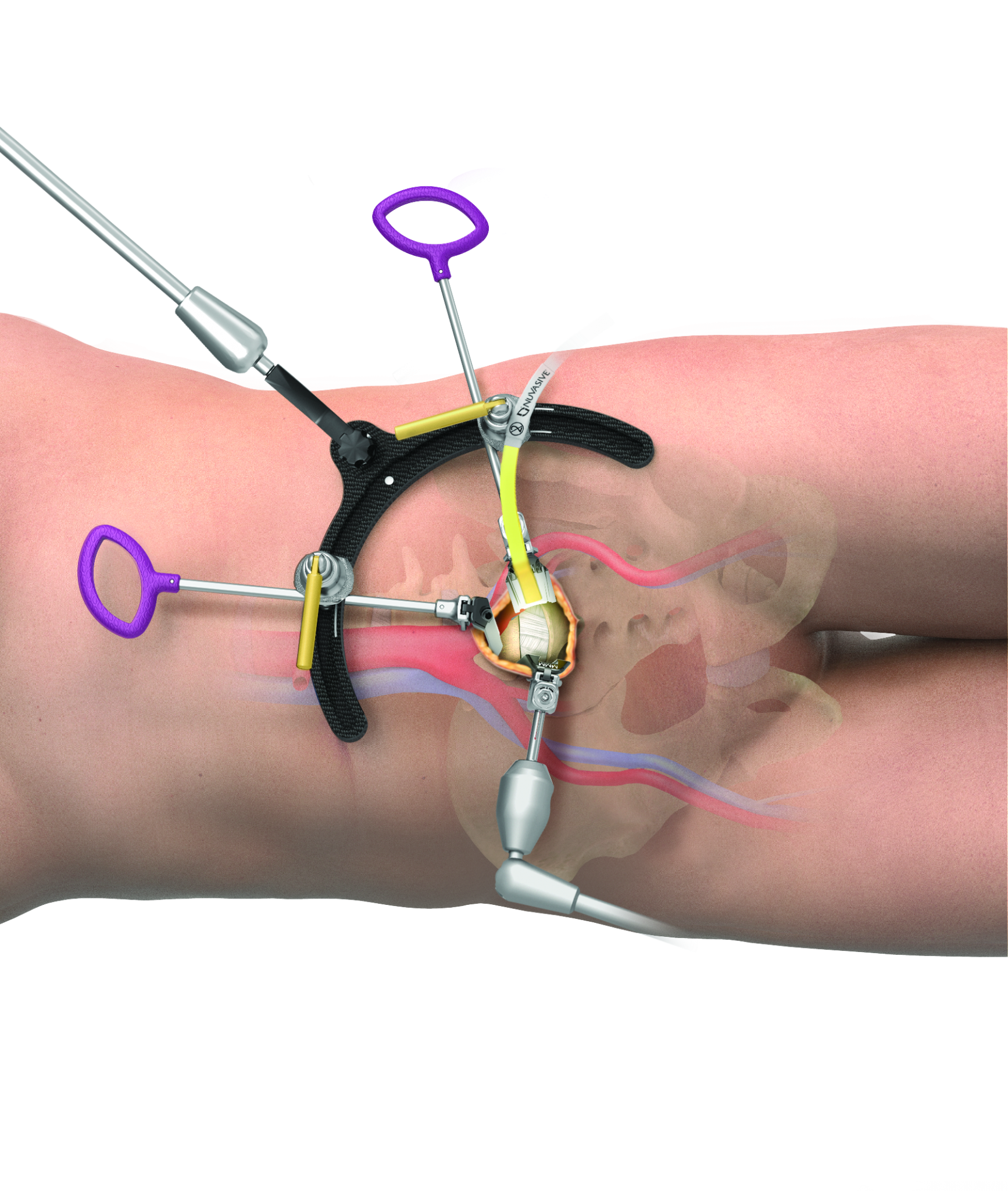
This new technique offers many advantages, both for the doctor and for the patient
2. Integration of 3D rotational angiography using GE Healthcare IGS 7 with Navigation (Stealth Station) from Medtronic
The IGS 7 system is a hybrid operating room and today is widely known to vascular surgeons. However, in other surgical disciplines, and more particularly in spinal surgery, its usage is limited.

Dr. van Schaik has worked with GE Healthcare and Medtronic on integrating 3D rotational angiography (GE Healthcare) with optical navigation (Medtronic) for placing screws and cages in back surgery.

One of the most valuable attributes of the Hybrid OR is its ability to generate high quality 3D images throughout the surgical procedure. High-definition CBCT is made easy with the IGS 7 wide-bore C-arm and large field-of-view detector for wide anatomical coverage in one fast spin. New additional degrees of freedom enable intra-operative CBCT even with table tilt and gantry translation, to perform imaging in complex patient positions. With IGS 7, the 3D rotational angiography produces slices which are compatible with the DICOM CT format for export to all major navigation systems such as Stealthstation.

Then, the surgeon can operate on the patient using optical navigation and benefitting from the High definition 3D images.
Now, both vascular surgeons and spinal surgeons can take full advantage of a single device with two high-performance modalities.
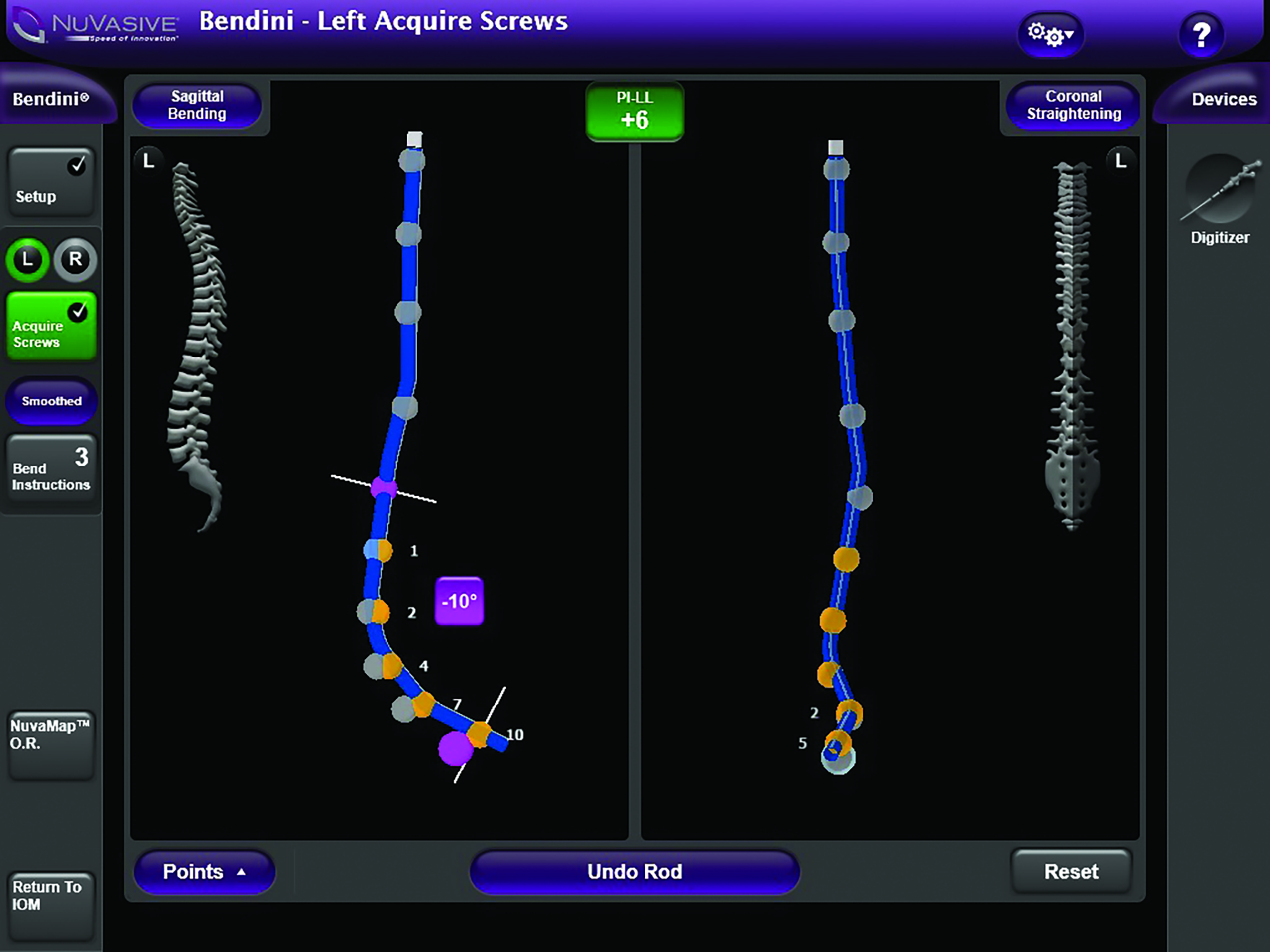
3. Rod bending techniques
Until recently, a major challenge when patients have to undergo back surgery in which several levels of the spine have to be fixed, was to bend the rod in the right way to fit properly in the screw heads. Thanks to a clever combination of various techniques, we can now have the computer calculate the rod bending and obtain an exactly correct folded bar.

The spinal rod bending system offers tools which can assist in complex degenerative deformity cases. The procedure is designed to benefit both surgeons and patients by providing intraoperative flexibility and restored alignment.
In 2017, we made the news because we were the first in Belgium to use this new technique during an operation. Result: decreased Operating Room Time, customization of the Rod, and less stress on the construct.
Unfortunately, we did not make the news fast enough with information that would be useful for a much larger group of people:
Prevention remains the key to success
A surgical procedure is often only one step in the treatment, afterwards a patient will have to continue working on their health (just like everybody else).

Testimonial of Ms. Najat Harrouch, patient of Dr. D. van Schaik.
Najat underwent an XALIF operation at level L5-S1 on February 20, 2020. Aged 34 at that time.
From June 2019 I started to have pain in my back and my legs. This pain was worsening every day especially as nightly leg cramps made sleeping hell.
I made an appointment with Dr. van Schaik who, in the first instance prescribed physiotherapy and MRI – CT and RX examinations.
After nine sessions of physiotherapy, the pain was still there and even worse.
Meanwhile the additional exams were performed and I had a new appointment with Dr. Van Schaik who took well over an hour to explain to me everything there was to see on the images from the exams. The cause was spondylolisthesis of the intervertebral disc. I had neurological complaints as a result of nerve entrapment and/or instability of the vertebrae. The explanation was in patient-friendly language.
According to Dr. van Schaik, an operation was necessary. Meanwhile he prescribed more advanced physiotherapy, but without improvement.
Before deciding on the surgery, I went for a second opinion. The second physician confirmed the diagnosis and the unavoidable operation, but recommended I undergo a series of peridural injections of cortisone. I did not follow that recommendation and returned to Dr. Van Schaik.
During this new consultation, Dr. Van Schaik took the time to explain the procedure and made an appointment for the surgery. He also gave me some literature and links to websites. Meanwhile I had an injection to kill the pain.
The day of the procedure, the doctor came to my room to ask how I felt and if I needed any additional information. But I knew exactly what was going to happen in the Operation room and when I would return to the room.
Shortly after the operation the physiotherapist urged me to get out of bed as soon as possible and to start walking. I also had the visit of an ergotherapist who explained to me how to handle daily tasks such as dressing myself, household chores, picking up things from the floor, climbing stairs, etc. After three days, I was discharged from the hospital.
The rehabilitation at home took approximately three months during which I trained intensively by walking (1 hour two or three times a day), climbing stairs and caring for the household. Now I feel extremely well and have absolutely no pain. However, this experience taught me to care for my back e.g. the way to get out of bed in the morning, bending the knees when picking up something, etc.
A while after the operation, Dr. van Schaik asked me if I would agree to coach patients who had to undergo the same operation. He explained to me that I am the living example that this kind of procedure has the expected result and, more importantly, that I can explain how the period after leaving the hospital works.
Since then, I have been a part of the “Experience Coaches” team.

SMALL STEPS AT A TIME WILL IMPROVE THE QUALITY OF YOUR LIFE!
We have a healthy obsession with time management, cost reduction, increased patient outcomes, reduction of complications, reducing re-admissions and increasing efficiency (in the operating room) and talking the language of the patient for their best possible understanding. All of these increases the quality of care.
My mission is that we, as care providers, should increasingly speak the same “language” with our patients and among each other.
As long as healthcare professionals remain too stuck in their own pigeonholes, change is still far away. That is why I am glad that more and more colleagues and caregivers realise that if we work together, everyone will benefit, especially the patient.
In the end the ultimate goal is: Bringing the patient back on track.